
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Trends in the Prevalence of Obesity and Its Phenotypes Based on the Korea National Health and Nutrition Examination Survey from 2007 to 2017 in Korea
- Sang Ouk Chin, You-Cheol Hwang, Hong-Yup Ahn, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2022;46(5):808-812. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0226
- 3,927 View
- 216 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study used data from the Korea National Health and Nutrition Examination Survey IV–VII from 2007 to identify the prevalence of obesity and its phenotypes (metabolically unhealthy obesity [MUO] and metabolically healthy obesity [MHO]) and their secular changes. The prevalence of obesity in Korea increased with significant secular changes observed (β=0.326, P trend <0.01) between 2007 and 2017, and especially in men (β=0.682, P trend <0.001) but not in women. The changes in the prevalence of obesity during the study period were different between men and women (P=0.001). The prevalence of MUO significantly increased only in men (β=0.565, P trend <0.01), while that of MHO increased only in women (β=0.179, P<0.05), especially in the younger age group (β=0.308, P<0.01).
-
Citations
Citations to this article as recorded by- Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Differences of Regional Fat Distribution Measured by Magnetic Resonance Imaging According to Obese Phenotype in Koreans
Ha-Neul Choi, Hyunjung Lim, Young-Seol Kim, Sang-Youl Rhee, Jung-Eun Yim
Metabolic Syndrome and Related Disorders.2022; 20(10): 551. CrossRef
- Hormonal Gut–Brain Signaling for the Treatment of Obesity
- Metabolic Risk/Epidemiology
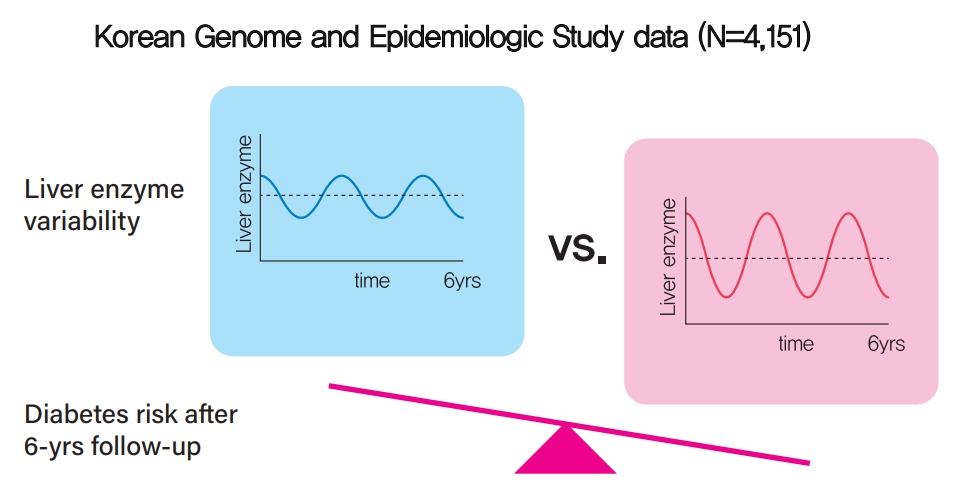
- Increased Visit-to-Visit Liver Enzyme Variability Is Associated with Incident Diabetes: A Community-Based 12-Year Prospective Cohort Study
- Kyuhoon Bang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
- Diabetes Metab J. 2021;45(6):890-898. Published online March 17, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0208
- 4,832 View
- 155 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 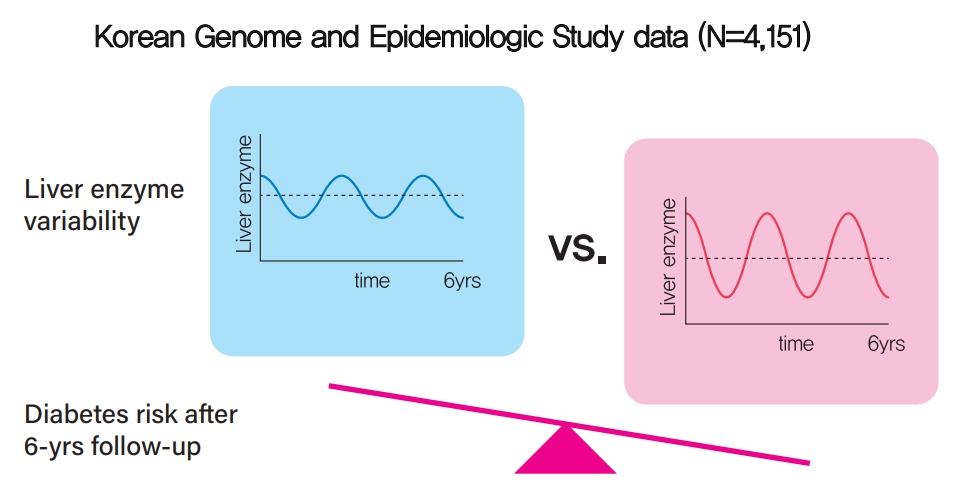
- Background
Fatty liver and/or increased liver enzyme values have been reported to be associated with incident diabetes. We sought to determine whether increased visit-to-visit liver enzyme variability is associated with incident diabetes.
Methods
Study participants were recruited from the Korean Genome and Epidemiologic Study (KoGES). A total of 4,151 people aged 40 to 69 years was recruited and tested every 2 years for up to 12 years. Visit-to-visit aspartate aminotransferase (AST) and alanine aminotransferase (ALT) variability was evaluated in first the 6-year period through the use of various variability measurements: standard deviation (SD), average successive variability, coefficient of variation (CV), and variation independent of mean (VIM). Oral glucose tolerance test was performed at every visit.
Results
During the 6-year follow‐up appointments, 13.0% (538/4,151) of people developed incident diabetes. Visit-to-visit AST variability was associated with an increased risk of diabetes independent of conventional risk factors for diabetes (hazard ratio per 1-SD increment [95% confidence interval]: 1.06 [1.00 to 1.11], 1.12 [1.04 to 1.21], and 1.13 [1.04 to 1.22] for SD, CV, and VIM, respectively; all P<0.05); however, no such associations were observed in the visit-to-visit ALT variability. According to alcohol consumption status, both AST and ALT variability were independent predictors for incident diabetes in subjects with heavy alcohol consumption; however, neither AST nor ALT variability was associated with diabetes risk in subjects who did not drink alcohol heavily.
Conclusion
Visit-to-visit liver enzyme variability is an independent predictor of incident diabetes. Such association was more evident in those who consumed significant amounts of alcohol.
- Clinical Diabetes & Therapeutics
- Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus
- You-Cheol Hwang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2019;43(5):582-589. Published online January 16, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0124
- 6,618 View
- 185 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The apolipoprotein B/A1 (apoB/A1) ratio is a stronger predictor of future cardiovascular disease than is the level of conventional lipids. Statin and ezetimibe combination therapy have shown additional cardioprotective effects over statin monotherapy.
Methods This was a single-center, randomized, open-label, active-controlled study in Korea. A total of 36 patients with type 2 diabetes mellitus were randomized to either rosuvastatin monotherapy (20 mg/day,
n =20) or rosuvastatin/ezetimibe (5 mg/10 mg/day,n =16) combination therapy for 6 weeks.Results After the 6-week treatment, low density lipoprotein cholesterol (LDL-C) and apoB reduction were comparable between the two groups (−94.3±15.4 and −62.0±20.9 mg/dL in the rosuvastatin group, −89.9±22.7 and −66.8±21.6 mg/dL in the rosuvastatin/ezetimibe group,
P =0.54 andP =0.86, respectively). In addition, change in apoB/A1 ratio (−0.44±0.16 in the rosuvastatin group and −0.47±0.25 in the rosuvastatin/ezetimibe group,P =0.58) did not differ between the two groups. On the other hand, triglyceride and free fatty acid (FFA) reductions were greater in the rosuvastatin/ezetimibe group than in the rosuvastatin group (−10.5 mg/dL [interquartile range (IQR), −37.5 to 29.5] and 0.0 µEq/L [IQR, −136.8 to 146.0] in the rosuvastatin group, −49.5 mg/dL [IQR, −108.5 to −27.5] and −170.5 µEq/L [IQR, −353.0 to 0.8] in the rosuvastatin/ezetimibe group,P =0.010 andP =0.049, respectively). Both treatments were generally well tolerated, and there were no differences in muscle or liver enzyme elevation.Conclusion A 6-week combination therapy of low-dose rosuvastatin and ezetimibe showed LDL-C, apoB, and apoB/A1 ratio reduction comparable to that of high-dose rosuvastatin monotherapy in patients with type 2 diabetes mellitus. Triglyceride and FFA reductions were greater with the combination therapy than with rosuvastatin monotherapy.
-
Citations
Citations to this article as recorded by- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
Yura Kang, Jung Mi Park, Sang-Hak Lee
Yonsei Medical Journal.2024; 65(1): 19. CrossRef - Combination Therapy of Ezetimibe and Rosuvastatin for Dyslipidemia: Current Insights
Maya R Chilbert, Dylan VanDuyn, Sara Salah, Collin M Clark, Qing Ma
Drug Design, Development and Therapy.2022; Volume 16: 2177. CrossRef - Ezetimibe and diabetes mellitus:a new strategy for lowering cholesterol
V.A. Serhiyenko, A.A. Serhiyenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(5): 302. CrossRef - The Effect of Rosuvastatin on Plasma/Serum Levels of High-Sensitivity C-Reactive Protein, Interleukin-6, and D-Dimer in People Living with Human Immunodeficiency Virus: A Systematic Review and Meta-Analysis
Akililu Alemu Ashuro, Yin-Guang Fan, Yuan-Sheng Fu, Dong-Sheng Di, Napoleon Bellua Sam, Hai-Feng Pan, Dong-Qing Ye
AIDS Research and Human Retroviruses.2021; 37(11): 821. CrossRef - Comparison of the Efficacy and Safety of Rosuvastatin/Ezetimibe Combination Therapy and Rosuvastatin Monotherapy on Lipoprotein in Patients With Type 2 Diabetes: Multicenter Randomized Controlled Study
Jiwoo Lee, You-Cheol Hwang, Woo Je Lee, Jong Chul Won, Kee-Ho Song, Cheol-Young Park, Kyu Jeung Ahn, Joong-Yeol Park
Diabetes Therapy.2020; 11(4): 859. CrossRef - Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Jaehyun Bae, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
Journal of Clinical Medicine.2020; 9(3): 798. CrossRef - Combined use of rosuvastatin and ezetimibe improves hepatic steatosis in patients with dyslipidemia
Won Dong Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Kwang-Hyub Han, Seung Up Kim
European Journal of Gastroenterology & Hepatology.2020; 32(12): 1538. CrossRef - Influence of rosuvastatin dose on total fatty acids and free fatty acids in plasma
Cristian I. Ciucanu, Sonia Olariu, Daliborca C. Vlad, Victor Dumitraşcu
Medicine.2020; 99(48): e23356. CrossRef - The effect of switching from statin-monotherapy to statin/ezetimibe combination therapy on lipid profiles in patients with type 2 diabetes and dyslipidemia: a multicenter open-label study (EUCLID)
Mitsuhide Takeshita, Atsushi Tanaka, Atsushi Kawaguchi, Keiko Sato, Shigeru Toyoda, Teruo Inoue, Koichi Node
Vascular Failure.2020; 4(1): 22. CrossRef - Response: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)
You-Cheol Hwang
Diabetes & Metabolism Journal.2019; 43(6): 915. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Changes in Plasma Free Fatty Acids Associated with Type-2 Diabetes
Amélie I. S. Sobczak, Claudia A. Blindauer, Alan J. Stewart
Nutrients.2019; 11(9): 2022. CrossRef
- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
- Risk Factors for the Progression of Intima-Media Thickness of Carotid Arteries: A 2-Year Follow-Up Study in Patients with Newly Diagnosed Type 2 Diabetes
- Sang Ouk Chin, Jin Kyung Hwang, Sang Youl Rhee, Suk Chon, You-Cheol Hwang, Seungjoon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong-taek Woo, Sung-Woon Kim, Young Seol Kim, Ja-Heon Kang, In-Kyung Jeong
- Diabetes Metab J. 2013;37(5):365-374. Published online October 17, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.5.365
- 4,782 View
- 31 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Intima-media thickness (IMT) of the carotid arteries is known to have a positive correlation with the risk of cardiovascular disease. This study was designed to identify risk factors affecting the progression of carotid IMT in patients with type 2 diabetes mellitus (T2DM).
Methods Patients with newly diagnosed T2DM with carotid IMT measurements were enrolled, and their clinical data and carotid IMT results at baseline and 2 years later were compared.
Results Of the 171 patients, 67.2% of males and 50.8% of females had abnormal baseline IMT of the left common carotid artery. At baseline, systolic blood pressure, body mass index and smoking in male participants, and fasting plasma glucose and glycated hemoglobin levels in females were significantly higher in patients with abnormal IMT than in those with normal IMT. Low density lipoprotein cholesterol (LDL-C) levels in males and high density lipoprotein cholesterol (HDL-C) levels in females at the 2-year follow-up were significantly different between the nonprogression and the progression groups. Reduction of the United Kingdom Prospective Diabetes Study (UKPDS) 10-year coronary heart disease (CHD) risk score after 2 years was generally higher in the nonprogression group than the progression group.
Conclusion LDL-C levels in males and HDL-C levels in females at the 2-year follow-up were significantly different between participants with and without progression of carotid IMT. Furthermore, a reduction in the UKPDS 10-year CHD risk score appeared to delay the advancement of atherosclerosis. Therefore, the importance of establishing the therapeutic goal of lipid profiles should be emphasized to prevent the progression of carotid IMT in newly diagnosed T2DM patients.
-
Citations
Citations to this article as recorded by- Comparison of the Effectiveness of Low Carbohydrate Versus Low Fat Diets, in Type 2 Diabetes: Systematic Review and Meta-Analysis of Randomized Controlled Trials
Tanefa A. Apekey, Maria J. Maynard, Monia Kittana, Setor K. Kunutsor
Nutrients.2022; 14(20): 4391. CrossRef Nomogram Based on Risk Factors for Type 2 Diabetes Mellitus Patients with Coronary Heart Disease
Rong Shi, Birong Wu, Zheyun Niu, Hui Sun, Fan Hu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 5025. CrossRef- HMGA1 Mediated High-Glucose-Induced Vascular Smooth Muscle Cell Proliferation in Diabetes Mellitus: Association Between PI3K/Akt Signaling and HMGA1 Expression
Qinghai Zhang, Ling Chen, Zhibo Zhao, Ying Wu, Jing Zhong, Gebo Wen, Renxian Cao, Xuyu Zu, Jianghua Liu
DNA and Cell Biology.2018; 37(4): 389. CrossRef - Relationship between frequency of hypoglycemic episodes and changes in carotid atherosclerosis in insulin-treated patients with type 2 diabetes mellitus
Tomoya Mita, Naoto Katakami, Toshihiko Shiraiwa, Hidenori Yoshii, Nobuichi Kuribayashi, Takeshi Osonoi, Hideaki Kaneto, Keisuke Kosugi, Yutaka Umayahara, Masahiko Gosho, Iichiro Shimomura, Hirotaka Watada
Scientific Reports.2017;[Epub] CrossRef - Impact of carotid atherosclerosis detection on physician and patient behavior in the management of type 2 diabetes mellitus: a prospective, observational, multicenter study
In-Kyung Jeong, Sin-Gon Kim, Dong Hyeok Cho, Chong Hwa Kim, Chul Sik Kim, Won-Young Lee, Kyu-Chang Won, Doo-Man Kim
BMC Cardiovascular Disorders.2016;[Epub] CrossRef - The effect of fibroblast growth factors and advanced glycation end-products on the intima-media complex thickness in patients with coronary heart disease and type 2 diabetes
Ekaterina Vladimirovna Ivannikova, Victor Yurievich Kalashnikov, Olga Mikhailovna Smirnova, Alexander Borisovich Kuznetsov, Сергей Anatolievich Terekhin, Alexander Viktorovich Il'in
Diabetes mellitus.2014; 17(2): 47. CrossRef
- Comparison of the Effectiveness of Low Carbohydrate Versus Low Fat Diets, in Type 2 Diabetes: Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Autoimmune Hypoglycemia in a Patient with Characterization of Insulin Receptor Autoantibodies
- Suk Chon, Moon Chan Choi, Yun Jung Lee, You Cheol Hwang, In-Kyung Jeong, Seungjoon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong-Taek Woo, Sung-Woon Kim, Jin-Woo Kim, Young Seol Kim
- Diabetes Metab J. 2011;35(1):80-85. Published online February 28, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.1.80
- 5,237 View
- 49 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Type B insulin resistance syndrome is a manifestation of autoantibodies to the insulin receptor that results in severe hyperglycemia and acanthosis nigricans. However, the mechanisms by which these autoantibodies induce hypoglycemia are largely unknown. In this paper, we report the case of patient with type B insulin resistance syndrome who presented with frequent severe fasting hypoglycemia and acanthosis nigricans.
Methods To evaluate the mechanism of hypoglycemia, we measured the inhibition of insulin binding to erythrocytes and IM9 lymphocytes in a sample of the patient's dialyzed serum before and after immunosuppressive therapy.
Results In the patient's pre-treatment serum IgG, the binding of 125I-insulin to erythrocytes was markedly inhibited in a dose-dependent manner until the cold insulin level reached 10-9 mol/L. We also observed dose-dependent inhibition of insulin binding to IM9 lymphocytes, which reached approximately 82% inhibition and persisted even when diluted 1:20. After treatment with glucocorticoids, insulin-erythrocyte binding activity returned to between 70% and 80% of normal, while the inhibition of insulin-lymphocyte binding was reduced by 17%.
Conclusion We treated a patient with type B insulin resistance syndrome showing recurrent fasting hypoglycemia with steroids and azathioprine. We characterized the patient's insulin receptor antibodies by measuring the inhibition of insulin binding.
-
Citations
Citations to this article as recorded by- Systematic Review—Type B Insulin Resistance With Isolated Hypoglycemia and Suppressed Insulin
Natasha Brown, Marianne S Elston
The Journal of Clinical Endocrinology & Metabolism.2024; 109(4): 936. CrossRef - Type B insulin resistance syndrome: a systematic review
Luizianne Mariano Martins, Virgínia Oliveira Fernandes, Manuela Montenegro Dias de Carvalho, Daniel Duarte Gadelha, Paulo Cruz de Queiroz, Renan Magalhães Montenegro
Archives of Endocrinology and Metabolism.2020;[Epub] CrossRef - Autoimmune hypoglycemia
Marina Y. Yukina, Diana A. Davtyan, Ekaterina A. Troshina, Nurana F. Nuralieva
Obesity and metabolism.2018; 15(3): 9. CrossRef - Unique pharmacology of a novel allosteric agonist/sensitizer insulin receptor monoclonal antibody
Simon A. Hinke, Anne M. Cieniewicz, Thomas Kirchner, Katharine D'Aquino, Rupesh Nanjunda, Jason Aligo, Robert Perkinson, Philip Cooper, Ken Boayke, Mark L. Chiu, Steve Jarantow, Eilyn R. Lacy, Yin Liang, Dana L. Johnson, Jean M. Whaley, Russell B. Lingham
Molecular Metabolism.2018; 10: 87. CrossRef - Combined Immunosuppressive Therapy Induces Remission in Patients With Severe Type B Insulin Resistance: A Prospective Cohort Study
Joanna Klubo-Gwiezdzinska, Maria Lange, Elaine Cochran, Robert K. Semple, Cornelia Gewert, Rebecca J. Brown, Phillip Gorden
Diabetes Care.2018; 41(11): 2353. CrossRef - Hypoinsulinemic Hypoglycemia Followed By The Onset Of Severe Insulin Resistance With Hyperglycemia And Circulating Anti-Insulin Receptor Antibodies In A Patient Suffering Systemic Lupus Erythematosus: A Case Report And Literature Review
Guillermo Martínez de Pinillos, Mariana Tomé, María M. Viloria, Joaquín Bobillo, María V. Cózar
AACE Clinical Case Reports.2017; 3(3): e284. CrossRef - The treatment of hyperinsulinemic hypoglycaemia in adults: an update
M. V. Davi′, A. Pia, V. Guarnotta, G. Pizza, A. Colao, A. Faggiano
Journal of Endocrinological Investigation.2017; 40(1): 9. CrossRef - Immunosuppressive Therapy in Treatment of Refractory Hypoglycemia in Type B Insulin Resistance: A Case Report
Lavanya Viswanathan, Imali Sirisena
Journal of the Endocrine Society.2017; 1(12): 1435. CrossRef - 反復する低血糖発作を契機に発見されたインスリン受容体異常症B型の1例(A case of type B insulin resistance presenting as recurrent hypoglycemia)
杉本 龍 (Ryu Sugimoto), 髙木 誠 (Makoto Takaki), 前原 潤一 (Junichi Maehara), 具嶋 泰弘 (Yasuhiro Gushima)
Nihon Kyukyu Igakukai Zasshi: Journal of Japanese Association for Acute Medicine.2017; 28(3): 100. CrossRef - Type B insulin resistance syndrome
Devina L. Willard, Mary Stevenson, Devin Steenkamp
Current Opinion in Endocrinology, Diabetes & Obesity.2016; 23(4): 318. CrossRef - Antibody-Mediated Insulin Resistance: When Insulin and Insulin Receptor Act as Autoantigens in Humans
Christelle Liminet, Julien Vouillarmet, Karim Chikh, Emmanuel Disse
Canadian Journal of Diabetes.2016; 40(5): 462. CrossRef - The insulin autoimmune syndrome (IAS) as a cause of hypoglycaemia: an update on the pathophysiology, biochemical investigations and diagnosis
Adel A.A. Ismail
Clinical Chemistry and Laboratory Medicine (CCLM).2016; 54(11): 1715. CrossRef - Type B insulin-resistance syndrome presenting as autoimmune hypoglycemia, associated with systemic lupus erythematosus and interstitial lung disease
Seon Mee Kang, Heung Yong Jin, Kyung Ae Lee, Ji Hyun Park, Hong Sun Baek, Tae Sun Park
The Korean Journal of Internal Medicine.2013; 28(1): 98. CrossRef - Treatment of recurrent hypoglycemia with plasmapheresis and steroid in nondiabetic patient
Mustafa Kulaksızoglu, Mustafa Sait Gonen, Levent Kebapcilar, Fatih Sahin, Fatih Demirci, Ali Topcu
Transfusion and Apheresis Science.2013; 48(1): 11. CrossRef - A Case of Persistent Hypoglycemia: When to Think Outside the Box
Yogeswari Venugopal, Shireene Vethakkan, Sargunan Sockalingam, Raja Jasmin, Karen Choong
Clinical Diabetes.2013; 31(3): 130. CrossRef - The effect of hyperglycemia and hypoglycemia on glucose transport and expression of glucose transporters in human lymphocytes B and T: An in vitro study
Bożenna Oleszczak, Leszek Szablewski, Monika Pliszka
Diabetes Research and Clinical Practice.2012; 96(2): 170. CrossRef - The effect of glucose concentrations in the medium on expression of insulin receptors in human lymphocytes B and T: anin vitrostudy
Bożenna Oleszczak, Leszek Szablewski, Monika Pliszka
Journal of Receptors and Signal Transduction.2012; 32(5): 263. CrossRef - Fulminant Type 1 diabetes in a pregnant woman as an initial manifestation of the insulin autoimmune syndrome
H. S. Kim, T.‐Y. Lee, E. Y. Kim, J. H. Choi, S. Y. Kim, Y.‐C. Hwang, J.‐H. Kang, K. J. Ahn, H. Y. Chung, I.‐K. Jeong
Diabetic Medicine.2012; 29(10): 1335. CrossRef - A Case of the Type B Insulin Resistance Syndrome with Chronic Hepatitis B
Hyun Seok Choi, Byoung Ho Choi, Seok Hoo Jeong, Shung Han Choi, Dong Su Shin, Sei hyun Kim, Young Sil Eom, Sihoon Lee, Yeun Sun Kim, Ie Byung Park, Ki Young Lee
Endocrinology and Metabolism.2011; 26(4): 360. CrossRef
- Systematic Review—Type B Insulin Resistance With Isolated Hypoglycemia and Suppressed Insulin
- The Changes in Early Phase Insulin Secretion in Newly Diagnosed, Drug Naive Korean Prediabetes Subjects
- Sang Youl Rhee, Joo Young Kim, Suk Chon, You Cheol Hwang, In Kyung Jeong, Seungjoon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong-taek Woo, Sung Woon Kim, Jin-Woo Kim, Young Seol Kim
- Korean Diabetes J. 2010;34(3):157-165. Published online June 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.3.157
- 4,545 View
- 28 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There have been no systematic observations regarding changes in early phase insulin secretion among Korean prediabetes and early stage type 2 diabetes mellitus (T2DM) patients.
Methods We conducted 75-g oral glucose tolerance tests (OGTT) in 873 subjects with suspected abnormal glucose tolerance. All subjects were diagnosed as having normal glucose tolerance (NGT), prediabetes (preDM), or T2DM according to the OGTT results and the insulin secretory and insulin resistance indices of each subject were calculated. Additionally, we analyzed the changes in early phase insulin secretion according to changes in fasting (Glc0), post-prandial (Glc120) glucose and HbA1c (A1c) levels.
Results As compared to subjects with NGT, the insulin secretory indices of the preDM and T2DM subjects progressively declined, and the insulin resistance indices were progressively aggravated. Early phase insulin secretion decreased rapidly according to the increments of Glc0, Glc120 and A1c, and these changes were most prominent in the NGT stage. Compared to the control group, the early phase insulin secretion levels of the preDM or T2DM subjects were less than 50% when Glc0 was over 100 mg/dL, Glc120 was over 145 mg/dL, and A1c was over 5.8%.
Conclusion This study suggests that progressive beta cell dysfunction in Koreans may be initiated and rapidly aggravated during the period generally designated as 'normal.'
-
Citations
Citations to this article as recorded by- Hospital-Based Korean Diabetes Prevention Study: A Prospective, Multi-Center, Randomized, Open-Label Controlled Study
Sang Youl Rhee, Suk Chon, Kyu Jeung Ahn, Jeong-Taek Woo
Diabetes & Metabolism Journal.2019; 43(1): 49. CrossRef - Differential role of insulin resistance and β-cell function in the development of prediabetes and diabetes in middle-aged and elderly Chinese population
Xueli Cai, Lili Xia, Yuesong Pan, Dian He, Huiping Zhu, Tiemin Wei, Yan He
Diabetology & Metabolic Syndrome.2019;[Epub] CrossRef - Effects of Primary Aldosteronism and Different Therapeutic Modalities on Glucose Metabolism
Mi Kyung Kwak, Jee Yang Lee, Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
Journal of Clinical Medicine.2019; 8(12): 2194. CrossRef - Insulin resistance increases the risk of incident type 2 diabetes mellitus in patients with non‐alcoholic fatty liver disease
Yuya Seko, Yoshio Sumida, Saiyu Tanaka, Kojiroh Mori, Hiroyoshi Taketani, Hiroshi Ishiba, Tasuku Hara, Akira Okajima, Atsushi Umemura, Taichiro Nishikawa, Kanji Yamaguchi, Michihisa Moriguchi, Kazuyuki Kanemasa, Kohichiroh Yasui, Shunsuke Imai, Keiji Shim
Hepatology Research.2018;[Epub] CrossRef - Longitudinal Changes in Insulin Resistance, Beta-Cell Function and Glucose Regulation Status in Prediabetes
Chul-Hee Kim, Hong-Kyu Kim, Eun-Hee Kim, Sung-Jin Bae, Jaewon Choe, Joong-Yeol Park
The American Journal of the Medical Sciences.2018; 355(1): 54. CrossRef - Prenatal Dexamethasone Exposure Programs the Development of the Pancreas and the Secretion of Insulin in Rats
Yu-Chieh Chen, Ying-Hua Huang, Jiunn-Ming Sheen, You-Lin Tain, Hong-Ren Yu, Chih-Cheng Chen, Miao-Meng Tiao, Ho-Chang Kuo, Li-Tung Huang
Pediatrics & Neonatology.2017; 58(2): 135. CrossRef - Insulin Secretory Capacity and Insulin Resistance in Korean Type 2 Diabetes Mellitus Patients
Jong-Dai Kim, Won-Young Lee
Endocrinology and Metabolism.2016; 31(3): 354. CrossRef - The effect of glargine versus glimepiride on pancreatic β-cell function in patients with type 2 diabetes uncontrolled on metformin monotherapy: open-label, randomized, controlled study
Jun Sung Moon, Kyoung Soo Ha, Ji Sung Yoon, Hyoung Woo Lee, Hyun Chul Lee, Kyu Chang Won
Acta Diabetologica.2014; 51(2): 277. CrossRef - Association of Obstructive Sleep Apnea and Glucose Metabolism in Subjects With or Without Obesity
Nan Hee Kim, Nam H. Cho, Chang-Ho Yun, Seung Ku Lee, Dae Wui Yoon, Hyun Joo Cho, Jae Hee Ahn, Ji A. Seo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Chol Shin
Diabetes Care.2013; 36(12): 3909. CrossRef - Relative contributions of insulin resistance and β‐cell dysfunction to the development of Type 2 diabetes in Koreans
C.‐H. Kim, H.‐K. Kim, E. H. Kim, S. J. Bae, J.‐Y. Park
Diabetic Medicine.2013; 30(9): 1075. CrossRef - Associations among Body Mass Index, Insulin Resistance, and Pancreatic β-Cell Function in Korean Patients with New-Onset Type 2 Diabetes
Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
The Korean Journal of Internal Medicine.2012; 27(1): 66. CrossRef - High normal HbA1c levels were associated with impaired insulin secretion without escalating insulin resistance in Japanese individuals: the Toranomon Hospital Health Management Center Study 8 (TOPICS 8)
Y. Heianza, Y. Arase, K. Fujihara, H. Tsuji, K. Saito, S. D. Hsieh, S. Kodama, H. Shimano, N. Yamada, S. Hara, H. Sone
Diabetic Medicine.2012; 29(10): 1285. CrossRef - The Prediabetic Period: Review of Clinical Aspects
Sang Youl Rhee, Jeong-Taek Woo
Diabetes & Metabolism Journal.2011; 35(2): 107. CrossRef - Predictive characteristics of patients achieving glycaemic control with insulin after sulfonylurea failure
Y.-H. Lee, B.-W. Lee, S. W. Chun, B. S. Cha, H. C. Lee
International Journal of Clinical Practice.2011; 65(10): 1076. CrossRef - Early Insulin Secretory Dysfunction in Korean Prediabetic Subjects: Should We Change the Criteria for "Prediabetes?"
Chul-Hee Kim
Korean Diabetes Journal.2010; 34(3): 154. CrossRef
- Hospital-Based Korean Diabetes Prevention Study: A Prospective, Multi-Center, Randomized, Open-Label Controlled Study
- Mutation Screening of HNF-1alpha Gene in Korean Women with Gestational Diabetes Mellitus.
- Hun Sung Kim, Sun Hee Hwang, Eun Sun Choi, So Young Park, Chang Hoon Yim, Ki Ok Han, Hyun Koo Yoon, Ho Yeon Chung, Kyung Seon Kim, Jeong Bok, Jong Young Lee, Sung Hoon Kim
- Korean Diabetes J. 2008;32(1):38-43. Published online February 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.1.38
- 2,479 View
- 21 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
S: Gestational diabetes mellitus (GDM) is defined as glucose intolerance with onset or first detection during pregnancy and mostly caused by insulin resistance and beta-cell dysfunction like type 2 diabetes. However, autoimmune or monogenic diabetes can contribute to GDM. Maturity-onset diabetes of the young (MODY) is a monogenic form of diabetes characterized by an early age of onset and an autosomal dominant pattern of inheritance. Most MODY cases are attributable to mutations in HNF-1alpha gene, also known as MODY3. We investigated whether mutations in HNF-1alpha gene are present in Korean women with GDM. METHODS: A total of 96 Korean women with GDM who have a family history of DM were screened for mutations in the HNF-1alpha gene. We evaluated the clinical characteristics of GDM women with HNF-1alpha gene mutations. RESULTS: Five of 96 patients (5.2%) were found to have a mutation in HNF-1alpha gene. Four of those (-23C > G, 833G > A (Arg278Gln), 923C > T, IVS5 + 106A > G) were novel and one (-124G > C) in promoter region was reported in previous study. The mean age of GDM women with mutations of HNF-1alpha gene was 34 years. Four women with MODY3 gene mutations required insulin therapy during pregnancy. GDM women with MODY3 gene mutations appeared to be decreased insulin secretion (HOMA-%B) than those without mutations. CONCLUSIONS: We have found the existence of MODY3 as well as novel HNF-1alpha gene mutations in Korean women with GDM. -
Citations
Citations to this article as recorded by
- Clinical Courses of Two Women with Gestational Diabetes Mellitus Who are GAD Antibody Positive.
- Sung Hoon Yu, Min Jun Song, Sung Hoon Kim, Chang Hoon Yim, Ki Ok Han, Won Kun Park, Hyun Koo Yoon, Ho Yeon Chung
- Korean Diabetes J. 2006;30(5):398-402. Published online September 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.5.398
- 2,150 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Gestational diabetes mellitus (GDM) is defined as glucose intolerance of various degrees with onset or first recognition during pregnancy. Women with GDM are at high risk of developing type 2 diabetes later in life, but the risk of developing type 1 diabetes is also increased. Positivity for glutamic acid decarboxylase (GAD) antibodies during pregnancy confers a high risk for subsequent progression to type 1 diabetes. Here, we reported the two cases with GDM who were GAD antibody positive and progressed to type 1 diabetes with different time-courses. One woman with GDM progressed rapidly to classical type 1 diabetes while the other became slowly progressive IDDM (SPIDDM) [or latent autoimmune diabetes in adults (LADA)].

 KDA
KDA
 First
First Prev
Prev





